Doha: From outbreak to pandemic to social isolation to quarantine, there are many terms associated with COVID-19 that can lead to confusion.
Making sure to have accurate information is key to understanding how and why it’s important to prevent the spread of COVID-19.
At several occasions the Ministry of Public Health, World Health Organisation and other institutions have continued to issue guidelines and explanations about several terms and actions.
Spread of disease
When a disease — and the virus that causes it —begins to spread, epidemiologists (who are considered the basic scientists of public health) take notice, looking for the frequency, patterns, and causes associated with it. Below are definitions of a few of those epidemiological terms that you may hear or see reported in the news, especially as they relate to COVID-19.

Endemic: The baseline, or expected, level of the disease in the community — meaning it always exists, like the common cold and flu, which are usually at low, predictable rates.
Epidemic: This refers to a sudden increase in the number of cases of a disease, above what is typically expected in a particular area. COVID-19 is thought to have reached epidemic proportions in China in mid-January.
Outbreak: This shares the same definition as epidemic, with one exception — an outbreak usually refers to a more limited geographic area.
Pandemic: An epidemic that has spread over several countries or continents, impacting many people. Pandemics typically happen when a new virus spreads easily among people who — because the virus is new to them — have little or no pre-existing immunity to it. COVID-19, which was declared a pandemic by the WHO in early March, is the first pandemic known to be caused by the emergence of a new coronavirus.
Cluster: A collection of cases occurring in the same place at the same time.
Community spread: Circulation of a disease among people in a certain area with no clear explanation of how they were infected — they did not travel to an affected area and had no close link to another confirmed case. This is sometimes referred to as community transmission.
Transmission: Although scientists are still learning about COVID-19 as more data becomes available, the virus is thought to be spread mainly from person-to-person contact, as well as w hen a person touches a surface or object that has the virus on it and then touches the mouth, nose, or possibly eyes.
Incubation period: The time between when a person is infected by a virus and when he or she notices symptoms of the disease. Estimates of the incubation period for COVID-19 range from 2-14 days, but doctors and researchers may adjust that as more data becomes available.
Droplet transmission: A form of direct transmission, this is a spray containing large, short-range aerosols (tiny particles suspended in air) produced by sneezing, coughing, or talking. Droplet transmission occurs — in general and for COVID-19 — when a person is in close contact with someone who has respiratory symptoms.
Asymptomatic: When a patient is a carrier of an illness but does not show symptoms. People are thought to be most contagious for COVID-19 when they are most symptomatic. Although researchers are still investigating how its spread might be possible at other times, including during the incubation period (called “pre-symptomatic transmission”) and even after symptoms have resolved.
Super-spreader: One person who, for unknown reasons, can infect an unusually large number of people. Infectious disease specialists say it is common for super-spreaders to play a large role in the transmission of viruses. In what’s known as the 80/20 rule, 20 percent of infected patients may drive 80 percent of transmissions.
Preventing COVID-19
As COVID-19 spreads across the country and the globe, there has been an increasing urgency—from individuals, scientists, doctors, and lawmakers at local, state, and national levels — for people to follow “best practice” prevention guidelines in an effort to stop or, at least, delay the spread of the disease. Below are commonly used terms to describe this effort.
Flattening the curve: Slowing the spread of the virus. If you map the number of COVID-19 cases over time, the expectation is that it will peak at some point — on a graph this peak would mirror a surge in hospital patients. “Flattening the curve,” which involves strategies to decrease transmission of the disease, would result in fewer patients during that peak period. This, in turn, would mean hospitals would be better able to manage the demands of patients who are sick with COVID-19 and other illnesses.
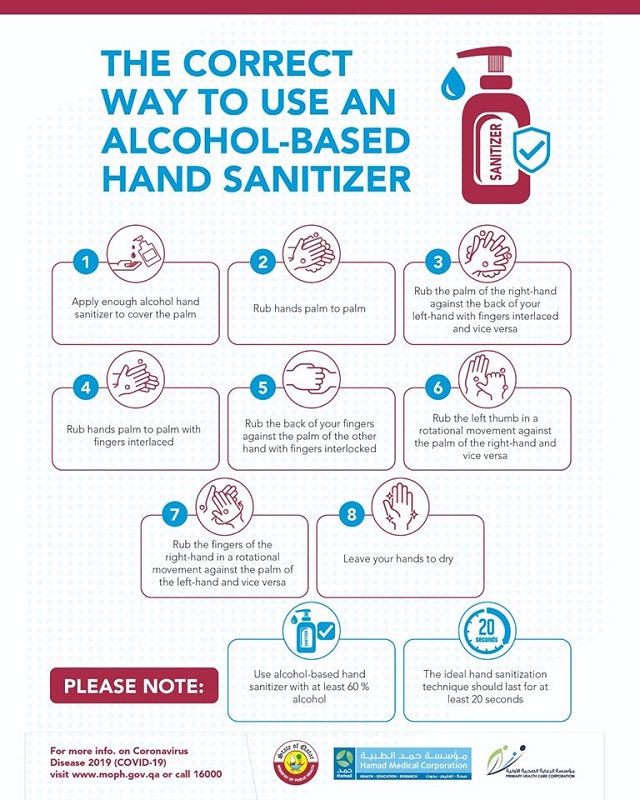
Hand hygiene: A key strategy for slowing the spread for COVID-19. Washing hands with soap and water for at least 20 seconds is one of the most important steps to take to protect against COVID-19 and many other diseases.
Social distancing: Putting physical distance between yourself and other people. This means avoiding groups of people (parties, crowds on sidewalks, lines in a store) and maintaining distance (approximately six feet) from others when possible. This is a key strategy for avoiding COVID-19 infection and to flatten the curve.
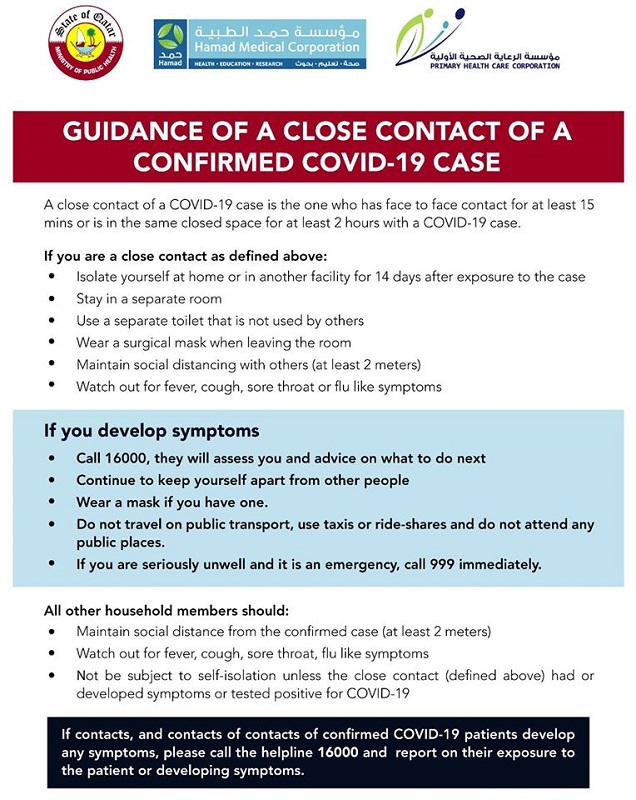
Self-isolation: Basically a voluntary agreement, this means you are to remain at home and not go to work or school. You’ll be expected to limit your movements outside (you can go for a walk and go shopping, though) and monitor your health for 14 days after returning from travel to a place known to have high numbers of COVID-19 infections.
Self-monitoring: This simply means checking yourself for COVID-19 symptoms, including fever, cough, or difficulty in breathing. If you notice symptoms, you should self-isolate and seek advice by telephone from a health care provider or local health department to determine whether you need a medical evaluation.
Isolation: On a larger scale, isolation involves keeping people with confirmed cases of a contagious disease separated from people who are not sick. If you have a confirmed case of COVID-19, for example, you may be put into isolation for public health purposes — it may be voluntary or compelled by federal, state, or local public health orders.
Quarantine: Unlike isolation, quarantine involves separating and restricting the movements of people who were exposed to a contagious disease to see if they become sick. The government may impose a quarantine on someone who was exposed to COVID-19 to avoid spread of the disease to others if they get sick.
The medical response: As the public does its part to help stop the spread of disease, health care workers on the front lines are caring for an increasing number of patients with COVID-19. The word “surge” is often used to describe the rapidly growing number of people in need of medical attention, a phenomenon that is already overwhelming hospitals around the country.
Drive-thru testing: Medical staff will take a “swab test” (usually done through the nose) to collect cells to test for COVID-19. These designated testing stations reduce the likelihood of further spreading the illness by allowing you to remain in your car, having the test taken through your open window. (The sample is then sent to a laboratory.) You will need an order from your primary care doctor before you can be tested for COVID-19, and tests are only available to people with symptoms.
Personal protective equipment (PPE): Specialised clothing or equipment, worn by an employee for protection against infectious materials, as defined by the Occupational Safety and Health Administration (OSHA). In health care settings, PPE may include gloves, gowns, aprons, masks, respirators, goggles, and face shields.




